Hemorrhoids: What Doctors Want You to Know But You’re Afraid to Ask

Hemorrhoids affect about 1 in 20 Americans, making them nowhere near as rare as you might think . People rarely talk about this condition, yet it becomes more common with age. The numbers show deal with it more than half of people over 50.
Hemorrhoids are swollen veins in your lower rectum . These swellings can show up inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids) . Your symptoms will change based on the type you have . External hemorrhoids bring anal itching, tender lumps near your anus, and pain that gets worse when you sit . Extra pressure from pregnancy, excess weight, or straining during bowel movements often triggers these uncomfortable swellings .
Most people shy away from learning about hemorrhoids because they feel embarrassed or scared. This piece will tell you everything doctors want you to know but you might hesitate to ask. You’ll learn to spot early symptoms, find treatments that work, and discover preventive steps that make a real difference.
Why people avoid talking about hemorrhoids
Hemorrhoids affect millions of Americans, yet people rarely talk about them. Most find it uncomfortable or downright mortifying to discuss problems with their anal region. Breaking this stigma starts with understanding why people avoid these conversations.
Embarrassment and stigma
People feel deeply uncomfortable talking about hemorrhoids[1]. Many suffer quietly and only seek help when the pain becomes unbearable—all because they feel ashamed. The natural hesitation to talk about private parts, especially those linked to bowel movements, creates a real barrier to getting treatment.
This shame goes beyond just talking about symptoms. People often wrongly link hemorrhoids to poor hygiene or sexual promiscuity [1]. These myths make a painful condition even harder to deal with emotionally.
The topic remains off-limits in everyday talk. As one medical source notes, “The mention of the word hemorrhoids can make you cringe with embarrassment… people don’t usually bring hemorrhoids up in casual conversation” [2]. This social barrier leaves many people without accurate information about this common condition.
Studies show that discomfort around “private parts” affects people from every background. Patients often try to ignore their symptoms or diagnose themselves rather than face what they see as humiliation—even with healthcare professionals [1].
Fear of diagnosis or treatment
The diagnostic process itself causes anxiety for many people. Just thinking about discussing bowel movements or having a rectal exam creates deep worry [1].
“Many patients worry that the process of diagnosis and treatment will be embarrassing or uncomfortable,” one gastroenterology source explains [1]. This worry can stop people from getting the medical help they need.
The possibility of a serious diagnosis scares some patients. Blood might signal hemorrhoids, but it could mean something more serious—which adds to people’s reluctance to see doctors [1]. This fear of bad news keeps many from making medical appointments.
Outdated ideas about treatment options make things worse. People imagine painful procedures when most cases need only minimal intervention [2].
Why early discussion matters
Avoiding medical help for hemorrhoids can lead to serious problems. “If left untreated, hemorrhoids can worsen over time,” one medical source cautions [3]. Minor discomfort can develop into a condition that needs advanced treatment.
Getting help early usually means simpler treatments work better. Healthcare providers stress that “” timely diagnosis and treatment are crucial in managing hemorrhoids effectively[1]. Delayed treatment often leads to more complex solutions.
Open conversations help correct false beliefs. Gastroenterologists deal with hemorrhoids every day—examining the rectum is as routine for them as checking an elbow injury [1]. This perspective helps reduce patient anxiety.
Breaking the silence around hemorrhoids helps spread awareness and education. Frank discussions about symptoms, triggers, and treatments enable people to take charge of their health [4]. This openness creates better support for everyone dealing with this common condition.
Your embarrassment and fear make sense, but don’t let them stop you from getting help. Healthcare providers treat many hemorrhoid cases each year [2]—you’re not alone, and there’s no reason to keep suffering without proper care.
What doctors want you to know about hemorrhoids
“The treatment of hemorrhoids is like a spectrum. There’s Preparation H, Tux and Witch Hazel on one side and then on the other side of that spectrum is the operating room.” — Dr. Sarah Umar, Gastroenterologist, Mayo Clinic, known as ‘Queen of Hemorrhoids’
Patients often walk into medical appointments with fears about hemorrhoids that make them expect the worst. Gastroenterologists and colorectal specialists have some surprising insights about this condition that could ease your mind.
Hemorrhoids are common and treatable
You’re not alone if hemorrhoids affect you. Studies from Korea, England, and Austria show of people had hemorrhoids between 14 and 39 percent[5]. About 10 million Americans reported hemorrhoid problems, which equals 4.4 percent of the population [5]. The numbers grow with age, and all but one of these people develop hemorrhoids by age 50 [1].
Medical professionals see hemorrhoids as a natural part of human anatomy. These become issues only when they grow larger or show symptoms. The outlook remains excellent in most cases.
“Most hemorrhoids resolve spontaneously or with conservative medical therapy alone,” note medical experts [5]. Treatment success rates bring good news. Non-surgical methods show a 10-50% recurrence over 5 years, while surgical hemorrhoidectomy has less than 5% [5]. Skilled surgeons report complications in fewer than 5% of cases [5].
They are not always painful
In stark comparison to this common belief, hemorrhoids don’t always hurt. Internal hemorrhoids grow inside the rectum above the dentate line. These lack cutaneous nerve endings, so they rarely cause discomfort [5]. Many people have them without any awareness.
“Internal hemorrhoids cannot cause cutaneous pain,” medical experts confirm [5]. These might cause bleeding during bowel movements without pain. Sometimes they prolapse or cause itching as a secondary effect [5].
Research on routine colorectal cancer screening patients revealed 39% had hemorrhoids. More than half of these patients showed no symptoms [1]. This proves hemorrhoids often exist without causing problems.
External hemorrhoids form under the skin near the anus. These sit in an area rich with pain-sensing nerves. Yet most cases show mild symptoms that respond well to basic treatments.
Most cases improve with simple care
Doctors share some good news – simple home treatments help most hemorrhoid cases. These usually clear up within a week [4].
Doctors suggest these home-based approaches:
- Increasing fiber intake (25 to 35 g per day) through diet and supplements
- Drinking plenty of fluids, especially water
- Taking warm sitz baths several times daily
- Using over-the-counter pain relievers like acetaminophen or ibuprofen
- Applying ice packs to reduce swelling
“Fiber supplementation decreases bleeding of hemorrhoids by 50% and improves overall symptoms,” according to medical research [1]. Warm water baths also help ease pain temporarily [1].
Doctors often recommend over-the-counter creams, ointments, suppositories, or pads that contain witch hazel, hydrocortisone, or lidocaine. These ingredients offer temporary relief from pain and itching [6]. Keep in mind that hydrocortisone can thin your skin after a week of use. Ask your healthcare provider about how long you should use it [6].
Recovery times bring more good news. “Most hemorrhoid symptoms improve within a week with at-home treatments,” medical experts note [7]. Contact your healthcare provider if symptoms persist beyond a week or if you notice severe pain or bleeding [6].
A tiny fraction of hemorrhoid patients need surgical removal [6]. This news relieves many patients who feared they might need invasive procedures.
Recognizing the symptoms early
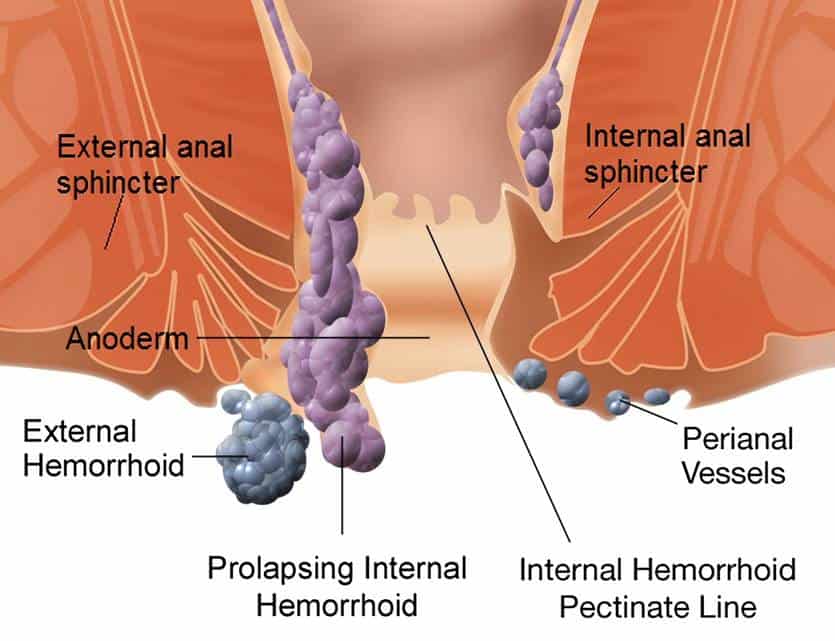
Image Source: en.wikipedia.org
Early detection of hemorrhoid symptoms helps you get quick treatment and avoid complications. You should know what signs to watch out that can make all the difference between minor discomfort and a serious medical emergency.
Internal vs external hemorrhoids symptoms
Internal and external hemorrhoids show different symptoms based on where they occur. in areas with fewer pain-sensing nerves Internal hemorrhoids develop inside the rectum[8]. You might not even notice them until they cause:
- Painless bright red bleeding during bowel movements
- Blood on toilet paper, in the toilet bowl, or streaked on stool
- A sensation of tissue sticking out from the anus (prolapse)
- Some itching or irritation around the anal area
Medical experts classify internal hemorrhoids by their prolapse level: Grade One (no prolapse), Grade Two (prolapse that goes back on its own), Grade Three (prolapse that needs manual pushing back), and Grade Four (prolapse that stays out) [3]. The symptoms become more noticeable with higher grades.
External hemorrhoids appear under the skin around the anus where many pain-sensing nerves exist [8]. These symptoms usually include:
- Itching or irritation around the anus
- Pain or discomfort that gets worse while sitting
- Swelling around the anal area
- Tender, sore lumps near the anus
- Bleeding after wiping [8]
External hemorrhoids look like soft lumps matching your skin color unless they form blood clots [8].
Bleeding hemorrhoids: when to worry
Bright red blood usually signals the first sign of hemorrhoids. The bleeding happens during bowel movements and shows up as small blood spots on toilet paper or in the bowl [9]. This bleeding might seem scary at first but rarely points to serious issues.
All the same, you should not assume rectal bleeding comes from hemorrhoids without proper medical evaluation [10]. These warning signs need immediate medical attention:
- Dark red blood (possibly from higher in the digestive tract)
- Heavy bleeding beyond a few drops
- Blood clots
- Bleeding with dizziness or lightheadedness
- Blood mixed with black or tar-like stool [11][12]
Patients under 40 with suspected hemorrhoid bleeding should see a doctor if they have warning signs like weight loss, stomach pain, fever, or anemia symptoms [10]. People over 40 need a complete colon check whatever their hemorrhoid status [10].
Signs of thrombosed hemorrhoids
inside an external hemorrhoid A thrombosed hemorrhoid happens when blood clots[13]. This painful condition shows clear signs that distinguish it from regular hemorrhoids:
- Sharp, sudden pain reaching its peak within 48-72 hours [3]
- A dark blue, purple, or black hard lump near the anus [14]
- Major swelling and inflammation [13]
- Extreme pain while sitting, walking, or during bowel movements [13]
The intense pain usually goes away after 4-5 days as your body absorbs the blood clot [3][14]. Medical care within the first 2-3 days gives the fastest relief through clot removal [10].
Sometimes thrombosed hemorrhoids get infected and cause fever [13]. You should contact your doctor right away if you notice fever or severe pain with a thrombosed hemorrhoid. Without treatment, infected thrombosed hemorrhoids can cause serious problems like perianal abscesses or anal fistulas [14].
Quick recognition of hemorrhoid symptoms leads to faster treatment. Most hemorrhoids respond well to basic home remedies, so early action helps reduce discomfort and prevent complications.
What really causes hemorrhoids?
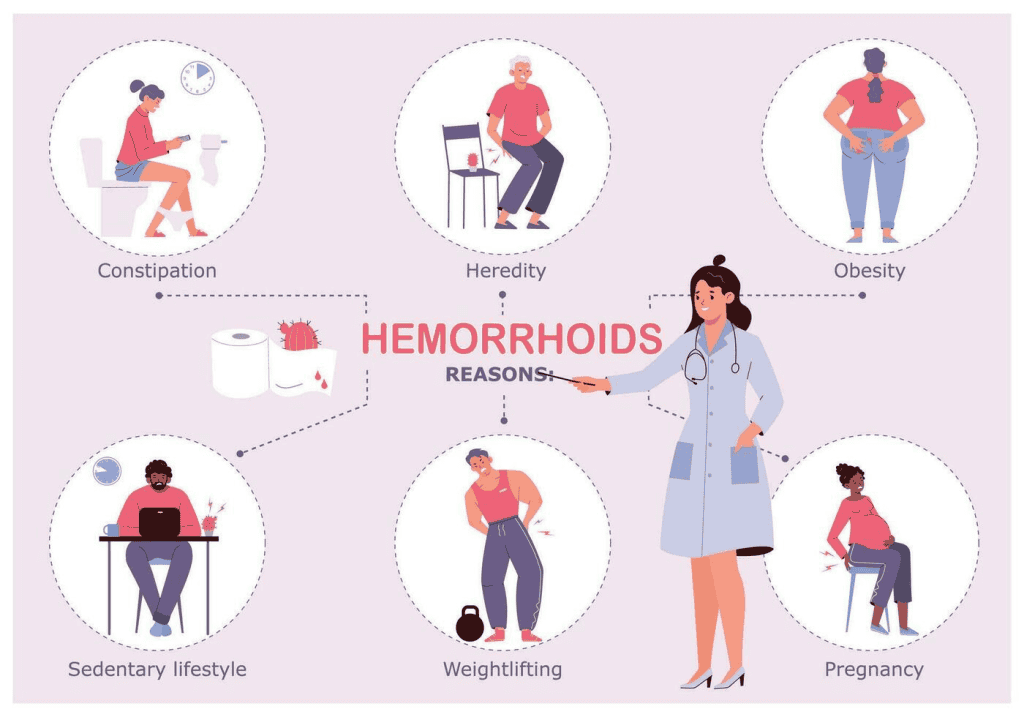
Image Source: Vecteezy
Learning about hemorrhoid triggers helps you prevent and manage this uncomfortable condition. The causes range from daily habits to biological factors you cannot control.
Lifestyle and dietary triggers
Your daily habits substantially influence hemorrhoid development. The veins around your anus stretch under pressure and may bulge or swell [2]. This pressure usually comes from:
- Straining during bowel movements
- Sitting for long periods, especially on the toilet
- Having chronic diarrhea or constipation
- Being overweight or obese
- Lifting heavy objects regularly
A low-fiber diet emerges as a major culprit [2]. Your stool becomes harder and more difficult to pass without enough fiber. This leads to increased straining during bowel movements. Fruits, vegetables, and whole grains provide high fiber—foods often missing from today’s diets [15].
Your rectum faces extra strain when you ignore the urge to use the restroom [15]. The extended time spent sitting on the toilet increases pressure on the anal area later. These conditions create an ideal environment for hemorrhoids to develop.
Pregnancy and hormonal changes
Pregnant women face a higher risk of developing hemorrhoids. Studies show that 25% to 35% of pregnant women experience this condition [16]. Some populations see hemorrhoids affect during the third trimester up to 85% of pregnancies[16].
Three key factors make pregnancy ideal for hemorrhoid development:
The growing fetus puts increasing pressure on your pelvic area and bowel [17]. This extra weight presses against your anal veins, which slows blood circulation and causes swelling.
Your blood volume increases substantially during pregnancy to support your developing baby [17]. Your veins must work harder to move more blood through your body.
Hormonal changes—particularly higher progesterone levels—make your vein walls relax and swell more easily [5]. This hormone also slows digestion, which often leads to constipation and worsens the problem [5].
These factors peak in the third trimester when your baby reaches its largest size [5].
Genetic and age-related factors
Your genes might make you more likely to develop hemorrhoids. A newer study, published by international researchers, found that add to hemorrhoid risk more than 100 regions in the human genome[1]. These genetic factors affect smooth muscle function, epithelial, and connective tissue [1].
Your family’s history often points to genetic predisposition. Genes for weaker colorectal muscles and connective tissue pass through generations in some families [18]. This inherited weakness makes these structures more vulnerable to damage over time.
Age plays an unavoidable role in hemorrhoid development. Your rectum’s and anus’s supporting tissues naturally weaken and stretch with age [2]. This explains why hemorrhoids become more common as you get older [19].
The risk increases with age, and hemorrhoids mostly affect people between 45 and 65 [20]. A large study found that 16.6% of people had hemorrhoidal disease, with slightly higher rates in females (17.2%) than males (16.3%) [19].
Knowledge of these causes explains hemorrhoid development and suggests prevention strategies. Many solutions involve simple lifestyle changes that counter these risk factors.
How long do hemorrhoids last and do they go away?
“How long will these hemorrhoids last?” People dealing with this uncomfortable condition often ask this question. The healing time varies based on the type, severity, and treatment approach.
Typical healing time
Minor hemorrhoid flare-ups resolve quickly for most people. Small hemorrhoids typically clear up without any treatment within a few days[7]. Hemorrhoid symptoms often disappear within a week when you use basic home treatments like sitz baths and over-the-counter medications [21].
Your hemorrhoids’ healing timeline depends on their type and severity:
- Internal hemorrhoids (Grade 1-2): These typically improve within a few days with proper self-care
- External hemorrhoids: Usually resolve within 1-2 weeks without intervention
- Thrombosed hemorrhoids: Pain typically peaks within 48-72 hours, then improves over 2-3 days as the body reabsorbs the blood clot [22]
- Post-surgical recovery: Following hemorrhoidectomy, expect a recovery period of 7-10 days [22]
Symptoms diminish gradually rather than disappearing suddenly. Bleeding usually stops first, followed by reduced swelling, while itching might last longer.
When symptoms persist
Many hemorrhoids resolve naturally, but persistent symptoms need attention. About half the people with hemorrhoids experience recurring symptoms [7]. A study found that , while nearly 55% needed hemorrhoidectomy for continuing symptoms only 13% of patients had no further trouble after an acute hemorrhoid episode[23].
You should contact your healthcare provider immediately if:
Your hemorrhoid symptoms don’t improve after a week of home treatment [21]. You experience severe pain or bleeding that doesn’t subside [21]. Your symptoms worsen instead of improving.
Healthcare providers point out that thrombosis is “merely an episode in the natural history of the disease and does not influence subsequent symptoms” [23]. This means you might develop recurring hemorrhoids without addressing the mechanisms, even after a painful thrombosed hemorrhoid heals.
Chronic vs acute hemorrhoids
One-time hemorrhoid flare-ups differ from chronic hemorrhoid disease. Acute hemorrhoids develop suddenly—perhaps after straining during constipation—and resolve within days or weeks.
Chronic hemorrhoids develop from persistent contributing factors or long-term habits [4]. These recurring hemorrhoids can affect sufferers for months or years without proper intervention.
The severity grade affects persistence and treatment outcomes. Grade 1 internal hemorrhoids (visible but don’t prolapse) heal faster than Grade 4 hemorrhoids (permanently prolapsed) [4]. Large external hemorrhoids take longer to heal than smaller ones [7].
Several factors increase your risk of developing chronic, long-lasting hemorrhoids:
- Sedentary lifestyle
- Insufficient dietary fiber
- Chronic constipation or diarrhea
- Regular straining during bowel movements [7]
Pregnancy-related hemorrhoids usually improve after childbirth [24], though women with multiple pregnancies face higher risks of chronic issues.
Most hemorrhoids eventually resolve, but addressing the mechanisms remains crucial to prevent recurrence. About 10-50% of hemorrhoids treated non-surgically recur within five years without lifestyle modifications [24].
Hemorrhoids self-care that actually works
You don’t always need to see a doctor to get relief from hemorrhoid discomfort. Most mild to moderate cases respond well to self-care methods that can ease symptoms and help you heal.
Using hemorrhoid creams and wipes
Over-the-counter hemorrhoid products provide quick relief from common symptoms. Products with , while witch hazel gives you a cooling, soothing effect hydrocortisone help reduce inflammation[25]. Options containing lidocaine can numb the area temporarily and ease pain [6].
The best hemorrhoid wipes are specifically medicated. These special wipes clean the area gently and deliver active ingredients that reduce irritation [26]. Preparation H, which doctors recommend most among OTC treatments, makes medicated wipes you can use before their cream or ointment to get better relief [27].
To apply:
- Clean the affected area first by gently wiping, patting, or blotting
- Put creams or ointments on external areas up to four times daily
- See your doctor if symptoms don’t improve within a week [6]
Note that you shouldn’t use steroid-containing products like Preparation H for more than a week. These can make your skin thin and break down if used too long [28].
Warm baths and cold compresses
Your comfort level improves a lot when you alternate between warm soaks and cold treatments. A warm sitz bath means sitting in a few inches of warm (not hot) water for 10-15 minutes, two to three times daily [25]. This therapy helps your sphincter muscle relax, boosts blood flow, and cuts down on itching and irritation [29].
A plastic sitz bath that fits over your toilet seat works well for many people, though your regular bathtub does the job too [28]. The hot water itself—not extras like Epsom salt—gives you the therapeutic benefit by easing pain, swelling, and muscle spasms [28].
Cold compresses help numb pain and reduce swelling between warm soaks. Put an ice pack wrapped in a towel (never direct ice) on the affected area for 5-10 minutes several times daily [6]. This works best for painful, swollen external hemorrhoids [8].
Hydration and fiber supplements
What you eat and drink affects your bowel movements directly. creates soft, regular bowel movements that reduce straining—this helps both prevent and treat hemorrhoids Getting enough fiber (25-30 grams daily)[25].
Supplements with psyllium (Metamucil) or methylcellulose (Citrucel) can help soften stool if you can’t get enough fiber from food [6]. Start adding fiber supplements slowly to avoid gas and bloating [25].
Water intake is just as vital as fiber. Drink at least 8-10 glasses daily to support digestion and prevent constipation [8]. Prune juice acts as a natural laxative and helps regulate bowel movements [6].
Most hemorrhoid symptoms get better within a week with consistent treatment [25]. You should see your healthcare provider if things don’t improve after seven days of home care, pain increases, or you notice bleeding [25].
When home remedies aren’t enough
Most hemorrhoid cases get better with home treatments. Medical professionals need to step in for some cases. Knowing the right time to get medical help can save you from unnecessary pain.
When to see a doctor
Your healthcare provider needs to know about these warning signs:
- Blood from your rectum that continues after a week of home care
- Pain that stays intense even with basic treatment
- A bump or swelling that stays the same
- Problems that affect your daily life
- Infection symptoms like fever, worse pain, or pus discharge
Blood that won’t stop needs medical attention right away. This could point to something more serious than hemorrhoids, like colorectal cancer or inflammatory bowel disease.
Minimally invasive treatments
Doctors suggest office procedures that don’t need hospital stays to treat severe or recurring hemorrhoids:
Rubber band ligation puts a small rubber band at the hemorrhoid’s base. This cuts off blood flow until the hemorrhoid shrinks and drops off. The procedure takes about five minutes and works 90% of the time on smaller hemorrhoids.
Sclerotherapy shrinks hemorrhoid tissue with an injected chemical solution. Patients need just 10-15 minutes for the procedure and recover quickly.
Infrared coagulation creates scar tissue with infrared light to stop blood flow to hemorrhoids. Patients feel almost no pain during this 10-minute treatment.
Surgical options and recovery
Some severe cases need surgery:
Hemorrhoidectomy removes problem tissue and works best for severe or recurring hemorrhoids. Recovery takes 2-3 weeks, and patients need strong pain medication.
Stapled hemorrhoidopexy (PPH) moves prolapsed tissue back and stops blood flow to hemorrhoids. Patients feel less pain than with regular hemorrhoidectomy and recover faster, usually within 7-10 days.
These surgical options work more than 95% of the time but might cause bleeding, infection, or hemorrhoids coming back. Your doctor can help you pick the treatment that fits your case at the time of consultation.
Living with hemorrhoids: lifestyle changes that help
“You should really shoot for 5 minutes or less on the toilet.” — Dr. Sarah Umar, Gastroenterologist, Mayo Clinic, known as ‘Queen of Hemorrhoids’
Small lifestyle changes can help manage hemorrhoids better in the long run. Your daily routine adjustments will make a big difference.
Exercise for hemorrhoids relief
Better blood flow from regular exercise helps reduce hemorrhoid symptoms [3]. The best choices are that don’t put pressure on your anal area. Your symptoms will improve with yoga poses like headstands, shoulder stands, and legs-against-the-wall positions low-impact exercises[3]. Swimming and water aerobics are great ways to work out multiple muscles while feeling soothed [3]. Stay away from activities that could make things worse, such as weightlifting, cycling, and rowing [30].
Healthy toilet habits
Listen to your body’s signals – holding it in leads to harder stools [31]. Keep your bathroom visits between 5-10 minutes to avoid extra pressure on your rectum [9]. A small footstool can raise your feet to create a natural squatting position. This straightens your rectum and makes bowel movements easier [11]. Clean up gently afterward with soft toilet paper or medicated wipes [31].
Long-term prevention strategies
Add to your diet through fruits, vegetables, and whole grains 25-30 grams of fiber[12]. Your stools will stay soft if you drink 6-8 glasses of water daily [21]. Desk job? Take breaks every hour to move around [32]. A standing desk or sit-stand workstation lets you change positions throughout your workday [3]. When you must sit for long periods, hemorrhoid pillows help reduce pressure [3].
Conclusion
Hemorrhoids can cause discomfort and embarrassment. Understanding this common condition enables you to take control of your health. Millions of Americans suffer from hemorrhoids, yet many avoid discussing their symptoms with healthcare providers because of social stigma or fear of diagnosis. Early detection and treatment improve outcomes by a lot and prevent complications.
Simple self-care measures work well for most hemorrhoid cases. You can manage symptoms and promote healing through warm sitz baths, over-the-counter creams, proper hydration, and more fiber intake. Making small lifestyle changes such as spending less time on the toilet, regular exercise, and healthy bowel habits will prevent future problems and provide lasting relief.
Of course, some cases need professional medical help. You should visit a doctor if you experience persistent bleeding, severe pain, or symptoms that don’t improve after a week of home treatment. Your healthcare provider can recommend minimally invasive procedures or surgical options that have excellent success rates.
Open discussions about hemorrhoids help normalize this condition that affects about half of all adults by age 50. Healthcare professionals treat hemorrhoids every day and can offer effective solutions without judgment. Your comfort and quality of life with this common condition depends on how quickly you address symptoms, take preventive steps, and get appropriate care when needed.
Key Takeaways
Understanding hemorrhoids can transform your approach to this common condition that affects half of adults over 50, helping you move from embarrassment to effective management.
• Hemorrhoids are extremely common and treatable – affecting 1 in 20 Americans with most cases resolving within a week using simple home remedies like sitz baths and fiber supplements.
• Early recognition prevents complications – internal hemorrhoids cause painless bleeding while external ones create painful lumps, but prompt treatment keeps symptoms manageable.
• Lifestyle changes offer lasting relief – increasing fiber to 25-30g daily, staying hydrated, limiting toilet time to 5 minutes, and regular exercise prevent recurrence better than any medication.
• Don’t suffer in silence due to embarrassment – doctors routinely treat hemorrhoids and consider discussing anal health as normal as addressing any other body part.
• Most cases never need surgery – only severe, recurring hemorrhoids require medical procedures, with 90%+ success rates for minimally invasive office treatments when home care isn’t enough.
The key to hemorrhoid management lies in understanding that this condition, while uncomfortable, responds exceptionally well to simple interventions. By addressing symptoms early and making basic lifestyle modifications, you can effectively manage hemorrhoids and prevent future flare-ups without letting embarrassment delay necessary care.
FAQs
Q1. How can I tell if I have hemorrhoids? Common signs include painless bleeding during bowel movements, itching or irritation around the anus, swelling near the anal area, and discomfort or pain, especially when sitting. If you experience these symptoms, it’s best to consult a healthcare provider for proper diagnosis and treatment.
Q2. Are hemorrhoids dangerous? Generally, hemorrhoids are not dangerous and often resolve on their own or with simple home treatments. However, they can cause discomfort and, in rare cases, lead to complications. If you experience severe pain, heavy bleeding, or symptoms that don’t improve after a week of home care, seek medical attention.
Q3. What’s the best way to prevent hemorrhoids? Prevention focuses on lifestyle changes. Increase your fiber intake to 25-30 grams daily, stay well-hydrated, exercise regularly, and avoid straining during bowel movements. Also, limit time spent sitting on the toilet and don’t ignore the urge to use the bathroom.
Q4. Can hemorrhoids go away on their own? Yes, many hemorrhoids, especially minor ones, can resolve on their own within a few days to a week. However, using home remedies like warm sitz baths, over-the-counter creams, and increasing fiber intake can speed up the healing process and provide relief from symptoms.
Q5. When should I see a doctor about hemorrhoids? Consult a healthcare provider if you experience persistent bleeding, severe pain, or if symptoms don’t improve after a week of home treatment. Also, seek immediate medical attention if you notice signs of infection such as fever or increasing pain, or if hemorrhoid symptoms interfere with your daily activities.
References
[1] – https://blog.23andme.com/articles/genetics-of-hemorrhoids
[2] – https://www.mayoclinic.org/diseases-conditions/hemorrhoids/symptoms-causes/syc-20360268
[3] – https://www.mintstl.com/blog/5-fundamental-lifestyle-changes-for-managing-hemorrhoids-at-home
[4] – https://www.ernestcastromd.com/blog/how-long-do-hemorrhoids-last
[5] – https://giassoc.org/pregnancy-and-hemorrhoids-understanding-the-causes-and-finding-relief/
[6] – https://www.webmd.com/digestive-disorders/hemorrrhoid-home-care
[7] – https://www.medicalnewstoday.com/articles/322976
[8] – https://www.drklause.com/blog/5-ways-to-ease-hemorrhoid-pain
[10] – https://www.aafp.org/pubs/afp/issues/2018/0201/p172.html
[11] – https://www.ranapileshospital.com/healthy-toilet-habits-to-avoid-hemorrhoids/
[12] – https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/eating-diet-nutrition
[13] – https://www.medicalnewstoday.com/articles/320407
[14] – https://www.verywellhealth.com/thrombosed-hemorrhoid-1945070
[15] – https://www.drklause.com/blog/bad-habits-that-cause-hemorrhoids
[16] – https://pmc.ncbi.nlm.nih.gov/articles/PMC2278306/
[17] – https://my.clevelandclinic.org/health/diseases/23498-pregnancy-hemorrhoids
[18] – https://www.adlermicromed.com/are-hemorrhoids-genetic/
[19] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8741788/
[20] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10641558/
[21] – https://www.mayoclinic.org/diseases-conditions/hemorrhoids/diagnosis-treatment/drc-20360280
[22] – https://www.preparationh.com/learn-more/how-long-do-hemorrhoids-last/
[23] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4473435/
[24] – https://www.manhattangastroenterology.com/how-long-hemorrhoids-last-when-to-see-a-doctor/
[25] – https://www.ucsfhealth.org/education/hemorrhoids
[26] – https://www.preparationh.com/products/medicated-portable-wipes/
[27] – https://www.preparationh.com/
[29] – https://my.clevelandclinic.org/health/treatments/24137-sitz-bath
[30] – https://orangecountyhemorrhoidclinic.com/best-and-worst-exercises-for-hemorrhoids/
[31] – https://www.preparationh.com/learn-more/using-the-bathroom/
[32] –https://veininstitute.com/5-lifestyle-tips-for-managing-hemorrhoids/

